
Automatically apply for jobs with Zippia
Upload your resume to get started.
Utilization review coordinator skills for your resume and career

15 utilization review coordinator skills for your resume and career
1. Patients
- Identified and accessed Medicare entitlement benefits for those patients who met eligibility requirements both prior to admission and during concurrent review.
- Coordinated the intensive Case Management program monitoring patients with high utilization to ensure appropriate outpatient care was obtained by the patient.
2. Patient Care
Patient care entails the diagnosis, recovery, and control of sickness as well as the maintenance of physical and emotional well-being through the use of healthcare providers' services. Patient care is described as services provided to patients by health practitioners or non-professionals under guidance.
- Coordinate with discharge planning through active organization and monitoring of the patient care process to promote continuity of care cost effectiveness
- Coordinate patient care between physicians and insurance companies, verify insurance protocol for inpatient hospital stays
3. Acute Care
The branch of secondary healthcare which is responsible for giving short-term care to patients recovering from severe injuries or urgent medical problems is known as acute care. Acute care comprises multiple domains like; emergency care, urgent care, short-term stabilization, pre-hospital care, critical care, and trauma care.
- Monitored acute care provided to members utilizing McKesson InterQual criteria.
- Conducted all diagnosis coding for the facility including, acute care SNF, rehab, E.R., short stay and ambulance.
4. Utilization Management
- Assist with utilization management quality assurance initiatives through participation in on-line log and/or case staffing with supervisor.
- Trained and consulted with staff on utilization management matters, assuring state and federal regulatory compliance.
5. Discharge Planning
- Identified quality concerns/appropriateness of inpatient medical necessity for HMO/POS members length of stay and facilitated discharge planning when appropriate.
- Work performance also included discharge planning during inpatient hospitalization and coordinating home health care services prior to hospital discharge.
Choose from 10+ customizable utilization review coordinator resume templates
Build a professional utilization review coordinator resume in minutes. Our AI resume writing assistant will guide you through every step of the process, and you can choose from 10+ resume templates to create your utilization review coordinator resume.7. Mental Health
Mental health is the state of wellbeing in which an individual can cope with the regular stresses and tensions of life, and can work productively without having any emotional or psychological breakdown. Mental health is essential for a person of any age and helps them make the right decisions in their life.
- Provided review of mental health treatment requests for inpatient to outpatient psychiatric care for military family members and retired military members.
- Peer reviewer for psychologists requesting approval for providing mental health treatment and psychological testing on an outpatient basis.
8. Home Health
- Utilize various sources to verify patient insurance eligibility for DME and Home Health Care.
- Initiated a joint venture with Home Health Services and Durable Medical Equipment Company.
9. Medicaid
- Participated in multiple outside agency surveys Medicaid Field Office, clinical reviews of internal processes and by other authorized government agencies.
- Reviewed Medicare and Medicaid patient records for quality of care, utilization of resources and appropriate assignment of Diagnosis Related Groups
10. Utilization Review
Another name for utilization review is utilization management. It is the process of ensuring that healthcare services are used in a suitable manner. Utilization review is a critical component of adding value to the health care system. Mostly, UR is carried out by healthcare insurance companies, but hospitals and other healthcare providers also perform the process. Utilization review has three types of assessment namely: concurrent, prospective, and retrospective.
- Prepared statistics and presented Medicare Regulations to various hospital department, including the Hospital Utilization Review Committee and Outpatient Advisory Committee.
- Performed utilization review for renowned eating disorder facility to en- sure quality and procure funds to fuel operations.
11. Appeals
- Conducted insurance appeals for treatment coverage via written and telephonic forms of communications.
- Prepared/correlated appeals for retroactive denials by third party players for appropriate committee action.
12. Concurrent Review
- Manage insurance process for 24-bed in-patient psychiatric facility including admission authorization, concurrent reviews, ECT authorization and Partial Hospitalization step-downs.
- Collaborated with attending physicians, concurrent review staff, social services and other ancillary providers.
13. Substance Abuse
- Monitored commercial insurance compliance with Pennsylvania state mandated benefits for substance abuse treatment.
- Work with third-party payers to ensure appropriate payment and utilization of Valley Hope substance abuse treatment services.
14. Data Entry
Data entry means entering data into a company's system with the help of a keyboard. A person responsible for entering data may also be asked to verify the authenticity of the data being entered. A person doing data entry must pay great attention to tiny details.
- Process included reviewing for medical necessity, criteria, benefit interpretation, insurance eligibility, and data entry.
- Research and data entry using multiple systems and complete tasks as assigned.
15. Outpatient Services
- Provide first level clinical review for all inpatient and outpatient services requiring authorization for assigned client group regarding:
- Monitored and authorized outpatient services according to established guidelines.
5 Utilization Review Coordinator resume examples
Build a professional utilization review coordinator resume in minutes. Browse through our resume examples to identify the best way to word your resume. Then choose from 5+ resume templates to create your utilization review coordinator resume.
What skills help Utilization Review Coordinators find jobs?
Tell us what job you are looking for, we’ll show you what skills employers want.
List of utilization review coordinator skills to add to your resume
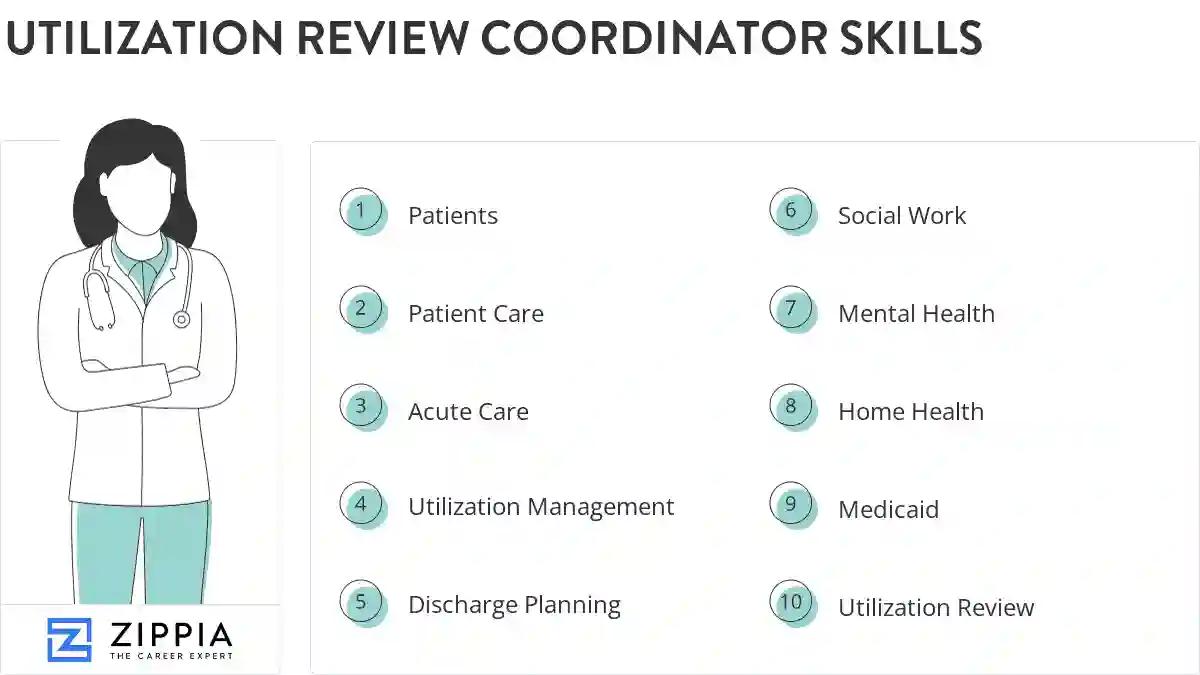
The most important skills for a utilization review coordinator resume and required skills for a utilization review coordinator to have include:
- Patients
- Patient Care
- Acute Care
- Utilization Management
- Discharge Planning
- Social Work
- Mental Health
- Home Health
- Medicaid
- Utilization Review
- Appeals
- Concurrent Review
- Substance Abuse
- Data Entry
- Outpatient Services
- Peer Review
- Rehabilitation
- Clinical Data
- Review Process
- Clinical Documentation
- CPT
- Medical Services
- CMS
- HIPAA
- Medical Necessity Criteria
- SNF
- Patient Charts
- Federal Regulations
- Hospital Admissions
- Chart Review
- Inpatient Admissions
- Interqual Criteria
- Insurance Benefits
- Retrospective Reviews
- Computer System
- Care Organizations
- ICD-9
- Durable Medical Equipment
- Milliman
- Clinical Review
- Hippa
- Eating Disorders
- Medical Documentation
- PHP
- DRG
- ASAM
- Private Insurance
- Medical Review
Updated January 8, 2025
6. Social Work